This is a link to a ten-minute video summary about birdshot chorioretinopathy given at the Birdshot Uveitis Day 2018 by Laura Steeples. It was recorded by NIHR Moorfields BRC and is on the Vimeo platform together with other presentations from the Day.
About birdshot chorioretinopathy
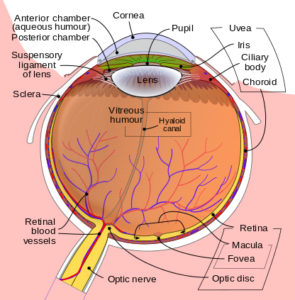
Birdshot chorioretinopathy or birdshot retinochoroidopathy (usually shortened to birdshot uveitis or birdshot) is a rare, potentially sight-threatening chronic posterior uveitis which usually affects both eyes. ‘Chronic’ means that it lasts a long time. ‘Posterior’ means that it affects the back of the eye. ‘Uveitis’ means inflammation of the uvea: the part of the eye that is made up of the iris, the choroid layer and the ciliary body. The uvea provides most of the blood supply to the retina, which is the light-sensitive tissue that lines the inner surface of the eye.
In the diagram of the eye below, you can see the position of the iris, the choroid and the ciliary body.
The first case of birdshot was described in 1949 by two ophthalmologists (eye specialists) Franceschetti and Babel, but it was not until 1980 that two other ophthalmologists, Ryan and Maumenee, coined the term ‘birdshot’ to describe the scatter pattern of the orange to cream-coloured retinal spots (lesions) seen in the condition. The pattern resembles that seen when pellets are fired from a shotgun.
There is a general view among many researchers and ophthalmologists that birdshot is a relatively new disease which had not occurred before the first description in 1949. This is because the symptoms, including the spots on the retina, are so striking that they would have been commented on by ophthalmologists if they had been observed before 1949.
What causes birdshot?
It is not known what causes birdshot. It is believed to be an autoimmune disease. An autoimmune disease is an illness that happens when the immune system, which normally keeps your body healthy, attacks your body’s own tissues.
The majority of people who are diagnosed with birdshot have inherited an antigen called HLA-A29. It is not yet known exactly what this means in relation to the functioning of the immune system. People who carry the HLA-A29 antigen may have an inherited defect in their immune system which makes them susceptible to developing birdshot. Research is being undertaken to try to clarify this.
However, many people carry the HLA-A29 antigen and never get birdshot, and some people develop birdshot but do not carry the HLA-A29 antigen. It is therefore assumed that other factors must trigger the disease. These triggers are elusive and have not yet been identified. A trigger might be, for example, an infection or some other environmental factor.
What are the symptoms of birdshot?
Usually, the initial symptoms of birdshot (and of many other forms of posterior uveitis) will be floaters and/or blurred vision caused by inflammatory cells in the vitreous humour, usually shortened to vitreous (see diagram). The presence of inflammatory cells in the vitreous is called vitritis.
In the initial stages, you are likely to have gradual, painless difficulty with seeing in one or both eyes. However, you may be able to continue to see well, and when your sight is tested (your visual acuity) it may show a good result.
Other symptoms may include:
- ‘Night blindness’ or difficulty seeing in dim light (nyctalopia)
- Problems with colour vision and difficulty distinguishing between certain colours (dyschromatopsia)
- Sensitivity to bright lights or glare (photophobia)
- Seeing flickering or flashing lights (photopsia)
- Distortions in vision (metamorphopsia)
- Fluctuating vision
- Pain in the eyes
- Decreased ability to judge depth
- Decreased peripheral (side) vision
- Shimmering vision (this is difficult to describe, but some people say it is like looking through dirty glass or through water)
- ‘Ceiling fan’ effect – when you close your eyes you are left with an image of a ceiling fan whirring round.
- If you have had birdshot for some time, an ophthalmologist is likely to be able to see the characteristic oval-shaped birdshot spots (lesions) on your retina at the back of your eyes.
Because birdshot is a rare disease, it can often be misdiagnosed or missed in its initial stages, particularly as the birdshot spots are often not clearly visible at first.
Who gets birdshot?
Because of the link to the HLA-A29 antigen, which is found more frequently in Caucasians than in other races, most people with birdshot are Caucasian. There does not seem to be a gender bias, although some ophthalmologists report diagnosing birdshot in more women than men.
In the past, it was believed that the average age when birdshot was likely to develop was 50 to 55 years and that it was a disease unlikely to affect people under the age of 35. However, people in their 20s and 30s are now being diagnosed with birdshot, and it may be that children can also suffer from it. It is important to remember this, as some specialists who do not often see people with birdshot may still believe that it occurs only in people in their 50s and older.
How many people have birdshot?
Birdshot is officially classified as a rare disease. A rare disease is defined in Europe as a disease affecting fewer than 5 per 10,000 of the population.
Because of its rarity and because it is a relatively newly recognised condition, it is difficult to identify how many people have been diagnosed with birdshot. The Birdshot Uveitis Society (BUS) has helped fund a UK surveillance study to try to establish accurate data on actual numbers of patients with birdshot.
What is the course (prognosis) of birdshot?
Birdshot seems to come in a range from mild to severe, from easy to treat to difficult to treat. Your treatment will depend on the amount of inflammation present in your eyes and on what is called the course of the disease, ie, how it progresses. Your ophthalmologist will continue to adjust your treatment according to how much your vision is affected by the inflammation.
The typical course of birdshot, like some other autoimmune diseases, is marked by flare-ups (exacerbations) of inflammation inside the eye which can cause loss of visual acuity if left untreated. Because of this, ophthalmologists believe in taking a proactive approach to treatment to ensure that inflammation is kept to a minimum and that the maximum amount of visual acuity can be preserved.
The most concerning issues relating to birdshot are that if it is severe and is left untreated, or if there are many flare-ups, this can lead to macular oedema. This is a swelling of the layers of eye tissue under the macula (see diagram) which can cause visual loss.
How is birdshot diagnosed?
Because birdshot is a rare condition that can be difficult to diagnose, it may be diagnosed through default – that is, tests for several other, more common, conditions that cause similar symptoms will be done before birdshot is considered. Usually, the final step in diagnosing birdshot will be made through a blood test to establish whether or not you test positive for the HLA-A29 antigen.
However, getting diagnosed and receiving appropriate medication can sometimes be difficult. This is because:
- many doctors and optometrists (opticians) will have never seen a case of birdshot
- there is still a belief amongst some ophthalmologists that birdshot is a self-limiting disease which will eventually go away or ‘burn out’
- newer forms of medication may be difficult to access in healthcare systems, including the NHS, as there is not a large amount of evidence to support their usefulness.
What tests will I have?
Tests include:
Fluorescein angiography (sometimes called fundus fluorescein angiography; FFA): (fluorescein – the type of dye that is used; angiography – a study of the blood vessels; fundus – the interior lining of the eye). This is an extremely valuable test that provides information about the eyes’ blood circulation and the condition of the back of your eyes. The test is done by injecting fluorescein dye into a vein in your arm. In just seconds, the dye travels to the blood vessels inside your eyes. A camera equipped with special filters that highlight the dye is used to photograph the fluorescein as it circulates though the blood vessels in the back of your eyes. If there are any circulation problems, swelling, leaking or abnormal blood vessels, the dye and its patterns will reveal these in the photographs. You will have yellow skin and yellow eyes for several hours after the test and your urine will be bright yellow. These effects are normal and will slowly disappear.
Indocyanine green angiography (ICG): this test is similar to fluorescein angiography. ICG angiography uses injected indocyanine green dye which is picked up (fluoresces) in infra-red light. Infra-red light wavelengths are able to penetrate the retinal layers, making the circulation in the deeper layers of the eye, particularly in the choroid (see diagram) visible when photographed with an infra-red sensitive camera.
Optical coherence tomography scan (OCT): this is a non-invasive (no injections needed) test used for imaging the retina, which is the multi-layered sensory tissue lining the back of your eye. This can show if you have any optic nerve damage or macular swelling (oedema). It can record tiny changes very accurately.
Electroretinogram (ERG): this is a series of non-invasive (no injections needed) tests where small wires are placed alongside your eyelids and receptors are placed on your forehead and the back of your head. You will then look at a range of flickering lights and patterns. This test checks how well you have maintained your eyesight – particularly in your retina and choroid – and checks the functioning of your rods and cones (the structures in your retina which pick up what you see). This test is painless, although you may find it slightly uncomfortable. For more information please see our ERG Factsheet.
Visual field test (perimetry; ‘fields’): this is a non-invasive (no injections needed) method of measuring your entire scope of vision: central and peripheral (side) vision. Visual field testing maps the visual field of each eye individually.
Is there a cure for birdshot?
At present, there is no known cure for birdshot. Most research being undertaken is looking at finding more effective medications that have fewer side-effects than those that are used now. However, there is also some research going on to establish the genetic links and the triggers for birdshot. This may lead to a cure or a prevention regime in the future.
Currently, the aim is to ensure that people with birdshot reach remission or stabilisation of their condition by using medications which can sometimes be difficult to tolerate and which need careful monitoring.
Much of the treatment for birdshot, therefore, has to rely on a very strong relationship between you and your ophthalmologist, with frequent contact and a willingness on the part of the ophthalmologist to listen to what you believe is going on in your eyes and a willingness to use newer forms of medication if the more traditional ones appear not to work.
What are the treatments for birdshot?
Your ophthalmologist will want to do two things: first, to reduce the inflammation in your eyes, and second, to work to control your immune system so that it stops attacking your eyes.
This is currently done by using a combination of corticosteroids (steroids) to reduce the inflammation in the back of your eyes, plus immunosuppressants to stop your immune system attacking your eyes. Steroids can be given either by mouth or directly into the eye by injection or implant. There is increasing use of steroids being placed into the eye to help control birdshot. Steroids and immunosuppressants are strong medications which have several side-effects, so it is important that you have regular medical supervision and check-ups (monitoring – see later). You may also need to take other medication to counteract any side-effects of the corticosteroids or immunosuppressants, particularly any effects on your stomach and your bones.
The goal of treatment is to find the lowest doses of medication that will allow you to maintain your eyesight and stabilise your birdshot, then allow you to reach remission.
Unfortunately, at the moment there is no single standard medication regime that works for everybody who has birdshot. Your treatment has to be tailored to suit you, and this may depend on the results of any of the tests you have had. If you have had a full range of tests before your diagnosis, you and your ophthalmologist will have a record of how your eyes are functioning. You will then each be in a good position to judge how well your medication is working.
If the first selected treatments prove unsuccessful and eye inflammation returns, there are other medications that can be used which may suit you better.
Who does the monitoring?
If you are taking immunosuppressants and steroids, your health will be monitored regularly, including monitoring for any unwanted side-effects.
In some eye clinics, the monitoring of your immunosuppressant treatment will be done by sending you to see a rheumatologist or a kidney (renal) specialist. This is because these doctors have experience in using immunosuppressant medications, which not every ophthalmologist has. It is important that you have reliable access to your monitoring and good communication between you, your GP, your ophthalmologist and, if applicable, your rheumatologist or renal specialist.
Your ophthalmologist or rheumatologist/renal specialist will advise what your monitoring should be and how often it should be done. It is important to follow your specialists’ instructions and get these tests done when they are due, as the testing is designed to safeguard your health.
Overall, the management of your treatment should aim to maximise your wellbeing on it and prevent unnecessary side-effects.
What are the monitoring tests?
Blood and urine tests check that your kidneys, liver and bone marrow are functioning well. Depending on which medications you are taking, your cholesterol levels or your blood pressure may be monitored. For some immunosuppressants, the blood levels of immunosuppressant (‘trough levels’) in your body have to be checked regularly to make sure you are not having too much or too little.
These monitoring tests are done very frequently to begin with, and then repeated between every six to twelve weeks, depending on the medication you take, the test itself, your test results and your ophthalmologist’s or other specialists’ advice. According to your eye clinic’s procedures, your tests may be done at your eye clinic, or by your GP, or by your local rheumatology/renal unit.
You are also likely to have repeated regular visual field tests, OCT scans and ERGs.
You may also be sent for further fluorescein and/or indocyanine green angiography.
Oral steroids, fracture risk assessment and DEXA (DXA) scans
If you are taking steroids by mouth, you should be assessed for your risks of damage to your bones (osteoporosis) and your fracture risk. If you are not offered this assessment, ask your doctors about it. The greatest rate of bone loss occurs during the first six to twelve months of taking steroids, so it is important to start any preventative treatment early. If you are likely to be taking steroids for three months or longer, which may happen in treating birdshot, your fracture risk assessment may mean that you are prescribed medication to help prevent bone loss. This is usually a medication from a class of medicines called bisphosphonates. Sometimes, calcium with vitamin D tablets may be prescribed for your bone health.
Depending on your assessed fracture risk, your ophthalmologist or your GP may arrange for you to receive a DEXA (dual energy X-ray absorptiometry) scan, also called a DXA (densitometry x-ray) scan. This scan assesses your bone density. Check with your doctors whether or not your assessed fracture risk means you should have a DEXA scan and if so, how often it needs to be repeated, as this does not happen automatically. For more information please see our DEXA Scan Factsheet.
Further information and support
Birdshot Uveitis Society (BUS) provides information and support to anyone with birdshot. We are setting up a birdshot patient database and biobank to help birdshot scientists and researchers.
Membership of BUS is free of charge. It allows you access to Birdshot Days held in the UK, where professionals and patients come together to exchange information.
Useful Birdshot Uveitis Society links
Please use this factsheet as background information to aid discussions with your doctors. Individual cases may vary enormously and so the best information will always come from your doctors.
The information in this factsheet was originally written for birdshot patients by birdshot patients in conjunction with Mr Nigel Hall, consultant ophthalmologist at University Hospital Southampton NHS Foundation Trust. It has been revised by clinician members of the National Birdshot Research Network.
If you want to print off a copy of this factsheet, please open up the following PDF link: Birdshot Uveitis Society factsheet
Revised March 2022